In the contemporary United States, access to abortion is shaped not only by clinical availability but by geography, logistics, and legal risk. Following major legal shifts that have allowed individual states to severely restrict abortion, increasing numbers of people are required to travel across state borders to access reproductive healthcare. Travel has therefore become a central—if unintended—component of the healthcare pathway, exposing deep inequalities in who can access care safely, affordably, and with dignity.
Against this backdrop, the Tubman Travel Project offers an instructive example of how community-based systems emerge when formal institutions withdraw or become inaccessible. The Project operates as an accompaniment and travel support initiative, assisting people—primarily women—to leave restrictive states and access abortion care elsewhere. Importantly, it does not treat travel as a purely logistical task, but as a social, emotional, and ethical process that can be intentionally designed.
From legal rights to lived access
Legal permission to access healthcare does not automatically translate into practical access. In states where abortion is banned or functionally inaccessible, individuals may face long travel distances, financial strain, legal uncertainty, and heightened emotional stress. These barriers disproportionately affect people who are young, low-income, undocumented, or otherwise marginalised.
Reproductive freedom travel highlights a central tension in rights-based systems: rights may exist in principle in one jurisdiction while being effectively unreachable in another. In this context, mobility becomes a proxy for access, transforming healthcare into a problem of transport, coordination, and safety rather than solely medical provision.
The Tubman Travel Project model
The Tubman Travel Project responds to this gap through a structured accompaniment model. Rather than leaving individuals to navigate travel alone, the Project coordinates group travel, vetted local support, and post-procedure care environments designed for rest and recovery. This includes transportation, safe handovers with trusted volunteers, and access to spaces where individuals can rest, eat, and recuperate before returning home.
This approach challenges dominant narratives that frame abortion travel as inherently traumatic. While acknowledging that travel under legal constraint is far from ideal, the Project demonstrates that with adequate care, preparation, and human support, the experience need not be defined solely by fear or distress. In some cases, shared travel has facilitated connection, solidarity, and ongoing mutual support among participants.
Accompaniment as infrastructure
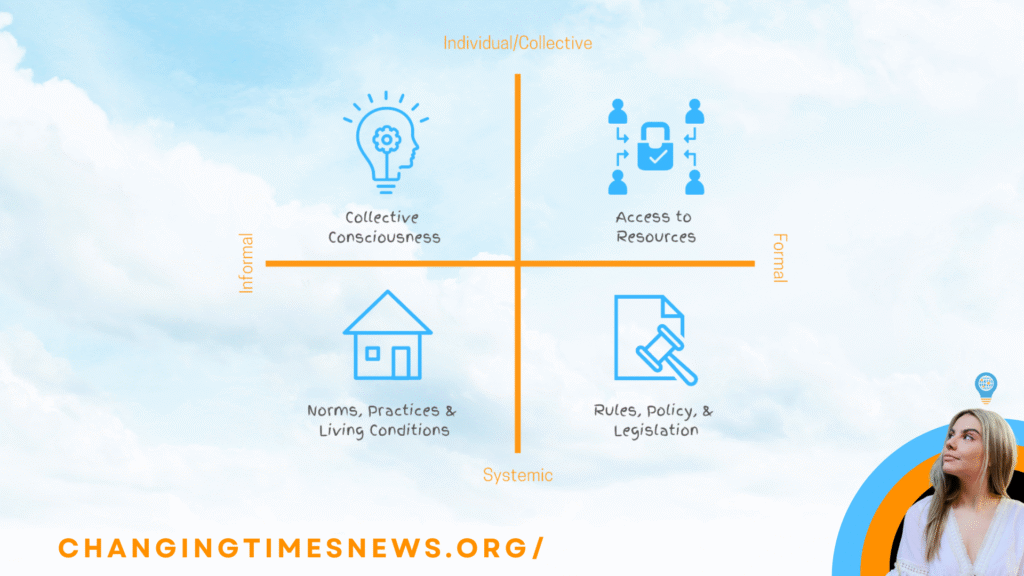
From a systems perspective, accompaniment functions as a form of social infrastructure. It redistributes risk from isolated individuals to collective systems and reduces the informational burden placed on those seeking care. By centralising knowledge—about routes, clinics, legal considerations, and recovery needs—the Project mitigates vulnerabilities that often arise when individuals must act alone under pressure.
Accompaniment also has preventative value. Structured support reduces exposure to misinformation, unsafe travel arrangements, and exploitation, particularly in environments where legal ambiguity creates opportunities for harm. In this sense, the Project operates at the intersection of healthcare access, harm reduction, and community organising.
Risk, legality, and movement sustainability
Reproductive freedom travel exists within a shifting legal landscape characterised by uncertainty and deterrence. Laws that enable civil liability or surveillance do not only target providers; they also shape the conditions under which support networks operate. For organisations like the Tubman Travel Project, this necessitates ongoing risk assessment, careful role allocation, and robust governance practices.
The Project’s leadership is explicit that direct-action support for contested rights has historically involved risk. Rather than eliminating risk entirely, the model seeks to distribute it responsibly, ensuring that individuals engage in roles aligned with their capacity and tolerance, while maintaining collective resilience.
Decentralisation and systems change
A notable feature of the Tubman Travel Project is its emphasis on decentralisation and replication. Rather than consolidating all expertise and responsibility in a single organisation or leader, the Project aims to train others to provide similar accompaniment in different locations. This distributed approach reflects an understanding of systems change as emergent rather than centrally engineered.
In systems theory terms, such decentralisation increases adaptability and reduces reliance on any single node. It allows new care systems to evolve in response to local conditions while remaining connected through shared principles and practices.
Broader implications
While the Tubman Travel Project is grounded in the specific legal and political context of the United States, the issues it addresses are not unique to that setting. Globally, access to healthcare is often mediated by geography, income, and social support rather than legal entitlement alone. The Project illustrates how communities respond when institutional guarantees erode—by building parallel systems that prioritise dignity, safety, and relational care.
Ultimately, reproductive freedom travel exposes a broader truth: access is not merely a matter of law or policy. It is a function of systems—human, logistical, and social—that either enable or obstruct people’s ability to exercise autonomy. The Tubman Travel Project demonstrates that, even under restrictive conditions, alternative systems of care can emerge, offering both immediate support and longer-term lessons for how access is made real in practice.